Background and Definitions
What is Revenue Cycle Management (RCM)?
What is a Denied Claim?
In healthcare, a claim is considered denied if the insurance company or payer determines that they will not pay for all or part of a medical service or procedure. This can happen for a variety of reasons, including: lack of medical necessity, exclusion from coverage, coding or billing errors, lack of pre-authorization and non-payment of premiums.
Industry Problems and Opportunities
Time and Resources - When a claim is denied, the healthcare provider or facility will usually receive an explanation from the insurance company detailing the reason for the denial. The provider may then have the option to appeal the decision, provide additional documentation or information, or adjust the billing and resubmit the claim. In addition, denied claims can also result in patient dissatisfaction, as patients may receive unexpected bills or have to wait longer for their claims to be processed and paid.
Financial Impact - Depending on the source, denials cost healthcare in the United States between $250 to $350 billion annually.
Open Market - Many denial solutions in the market, but not a clear leader in the industry. Those who offered a denial solution, targeted larger health care corporations with prices that would be out of range for mid to smaller practices.
Customers and Users
In a healthcare provider's office, denials are typically handled by the claims follow-up or billing department. Part of this department’s responsibilities include following up with insurance companies or payers to resolve any issues or denials.
The specific role or job title of the person who handles claims follow-up may vary depending on the size and structure of the healthcare provider's office. In smaller offices, it may be a billing specialist or a medical coder who handles claims follow-up, while in larger organizations, there may be dedicated teams or managers who oversee the RCM process.
Research, Approach and Iterations
Research & Analysis
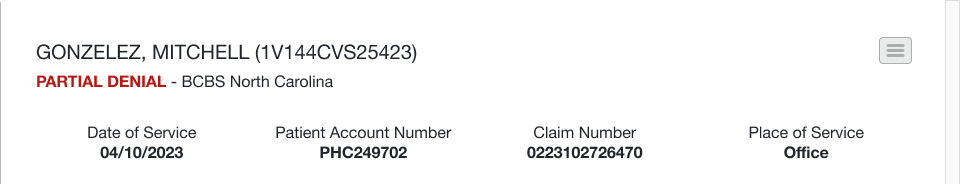
By examining numerous claims, the team identified recurring reasons for claim denials by payers. Based on their findings, they developed distinct categories and segments to classify and categorize denied claims into specific groups.
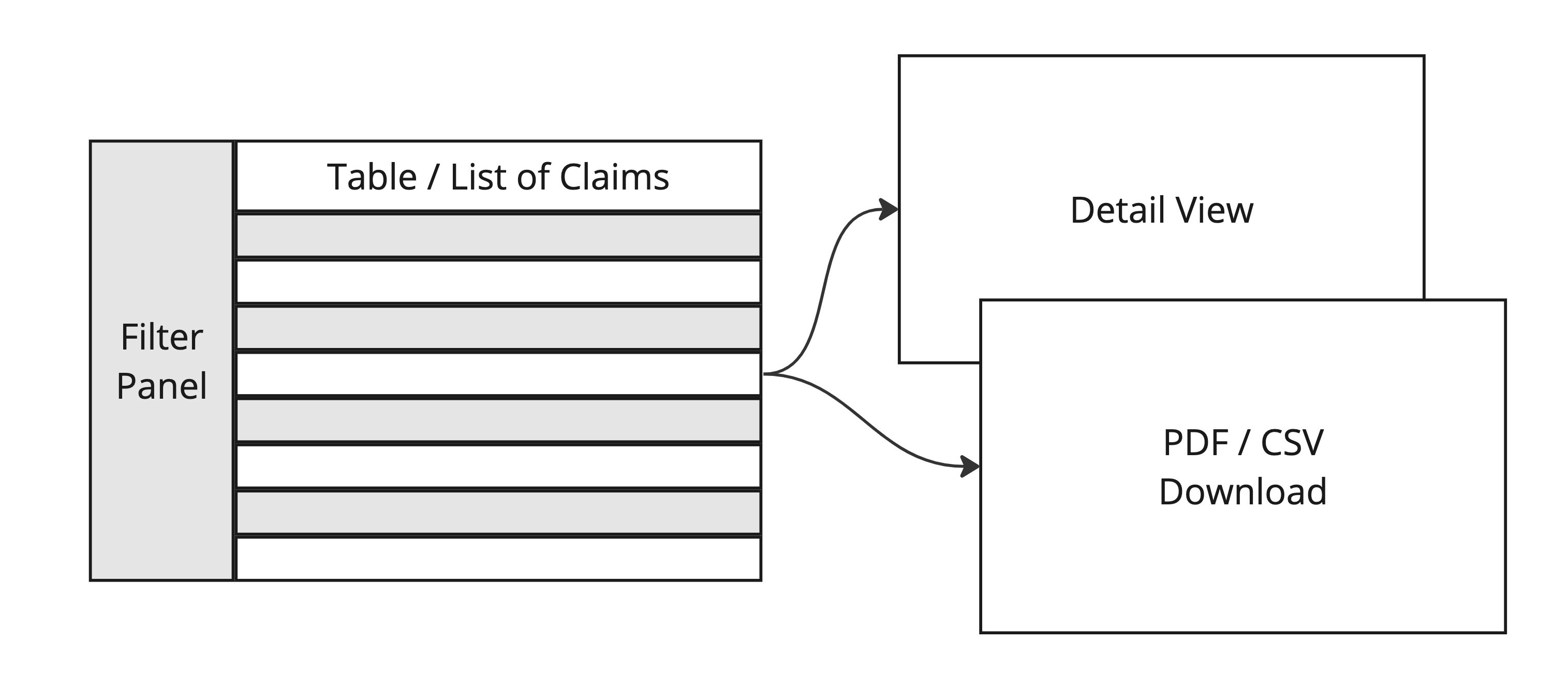
In other sections of the RCM application, data was typically presented in a tabular format with options for filtering, navigating to a detailed view, or downloading a PDF.
A New Approach
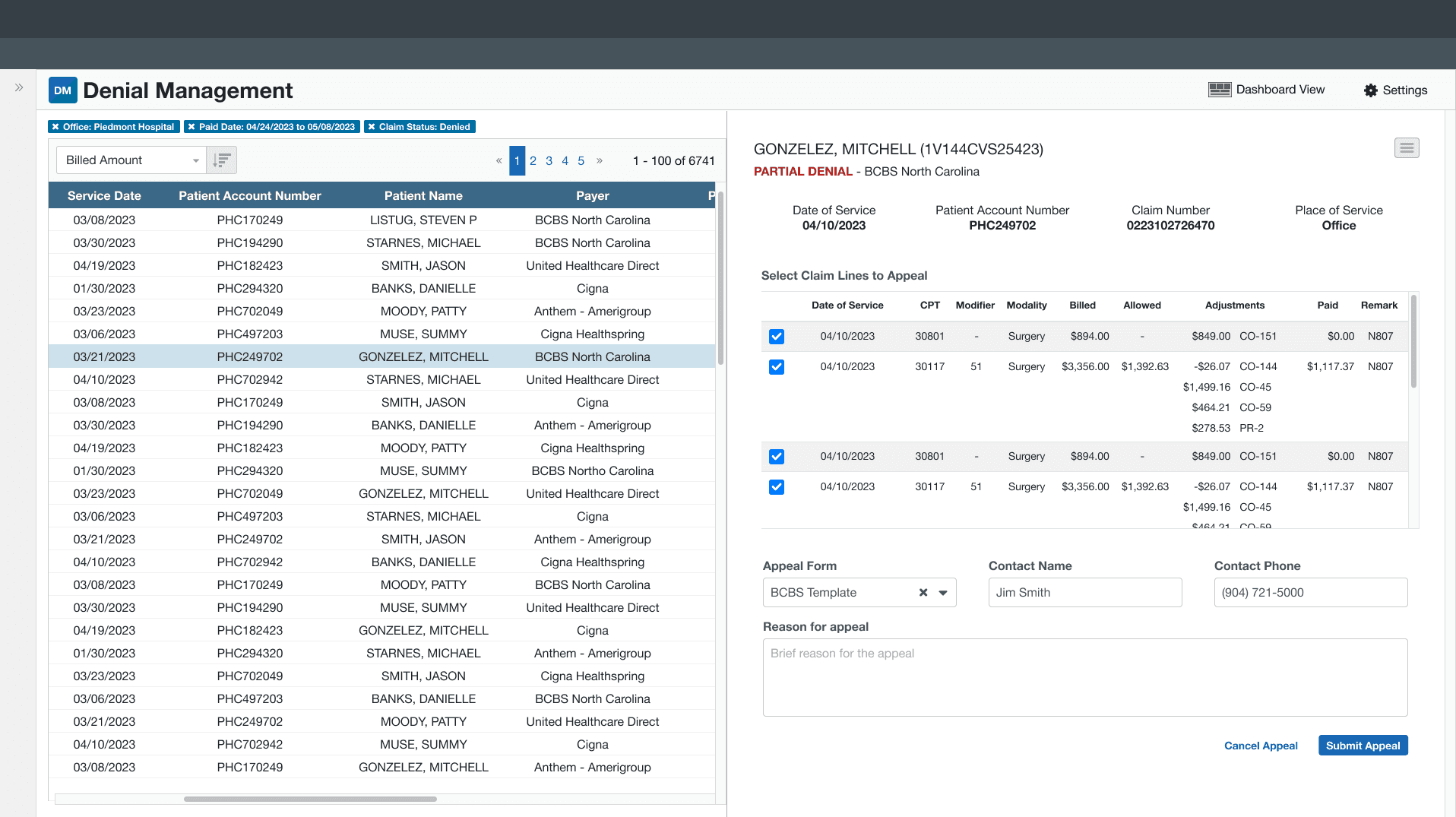
In our new prototype, we introduced a new detail panel that enables users to view and scroll through claim details on a split screen, resembling the interface of an email client.
Reduce Time
Upon reviewing the details, providers may wish to dispute the reason for the denial. To facilitate this, the team compiled a database containing hundreds of payer claim appeal forms. The goal was to simplify the process for providers by helping them quickly locate the appropriate form, ultimately reducing errors and saving time.
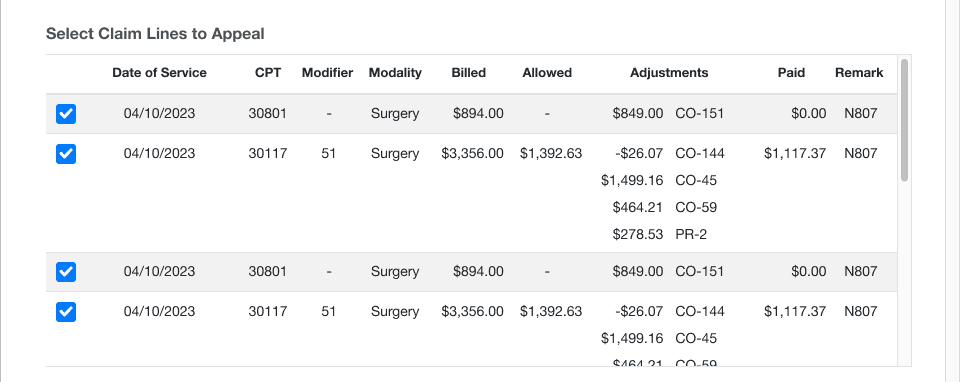
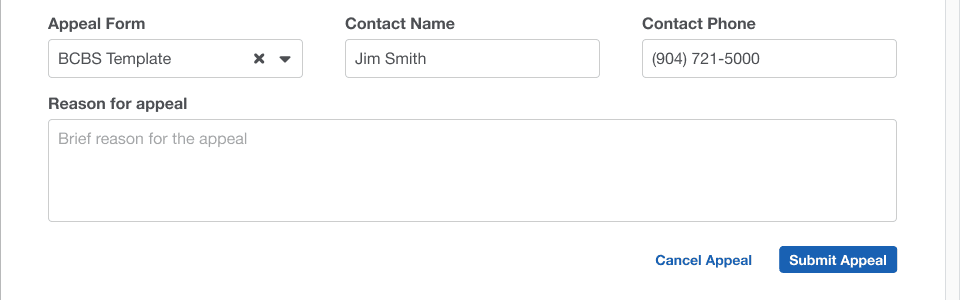
Additionally, we incorporated a feedback mechanism to gather input from users and ensure the database remains up-to-date, such as identifying missing or outdated forms.
Iterations and Adjustments
User Feedback
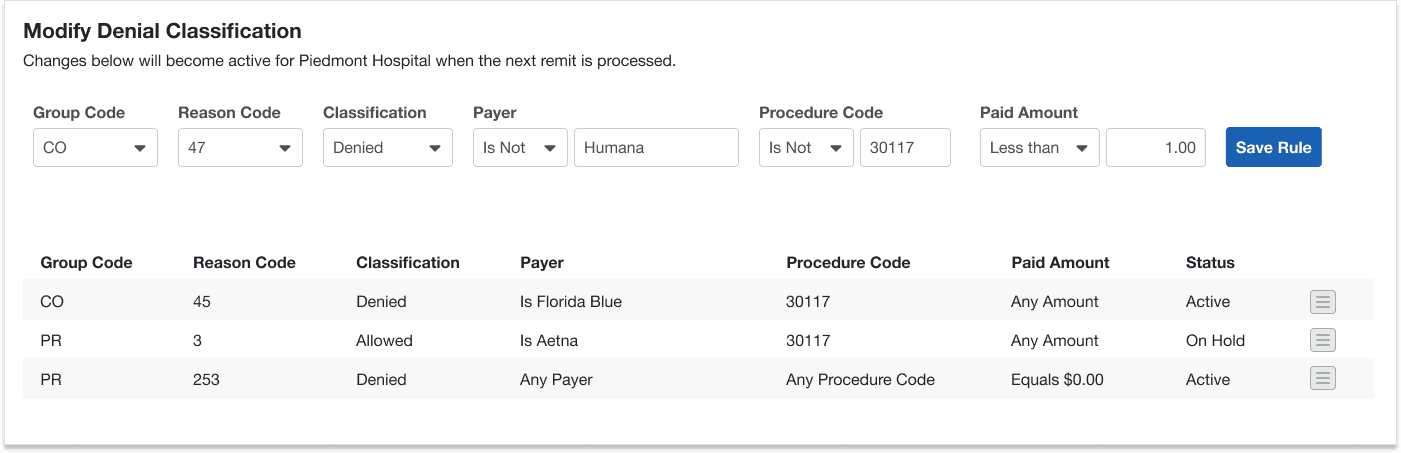
Overall, our users expressed enthusiasm for the new denial management module, particularly appreciating the addition of the detail panel and the ease of accessing appeal forms. However, one recurring piece of feedback we received from all users was the desire for greater control over what qualifies as a denied claim. From this feedback, we created two new features: customizable denial rules and a dashboard view to help identify trends or problem areas.
Making up the Rules
Our reasoning for categorizing a claim as denied was widely accepted, but opinions differed on which denials should be addressed first. To accommodate this, we granted users access to label claims as either 'Allowed' or 'Not Denied', and permitted them to re-label claims we had previously categorized as 'Allowed' to 'Denied'.
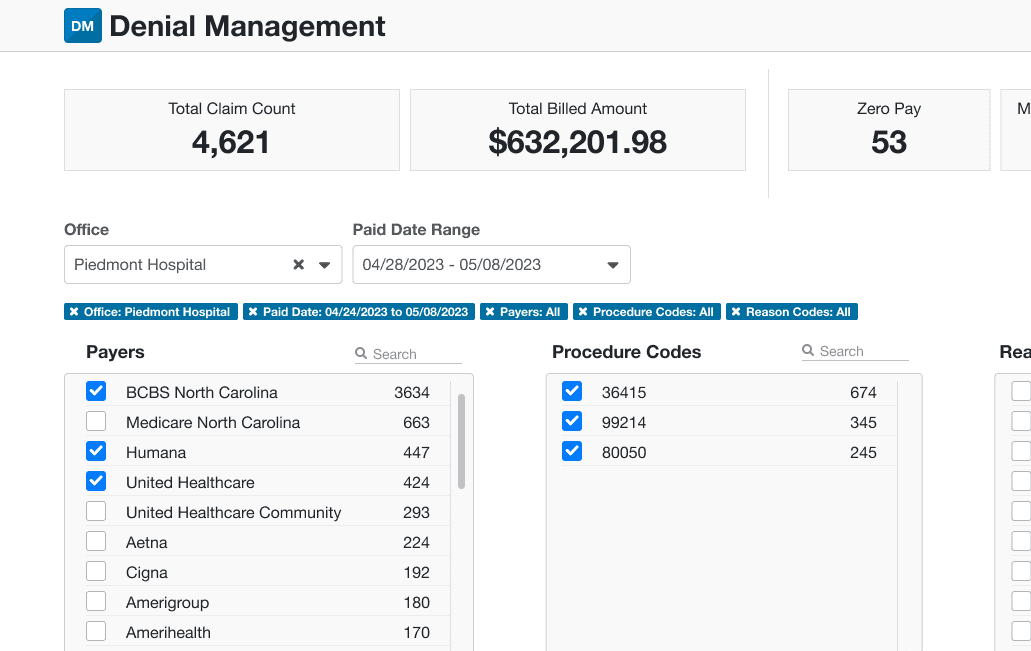
Looking at it differently
We noticed that in larger practices, even after applying customized rules and filtering down to a single day, thousands of denied claims were still being returned due to their high volume. Sorting and prioritizing denials in the current layout was overwhelming. To address this, we devised a two-part solution. Firstly, we used the same claim data that populated the tabular layout to create a dashboard view.
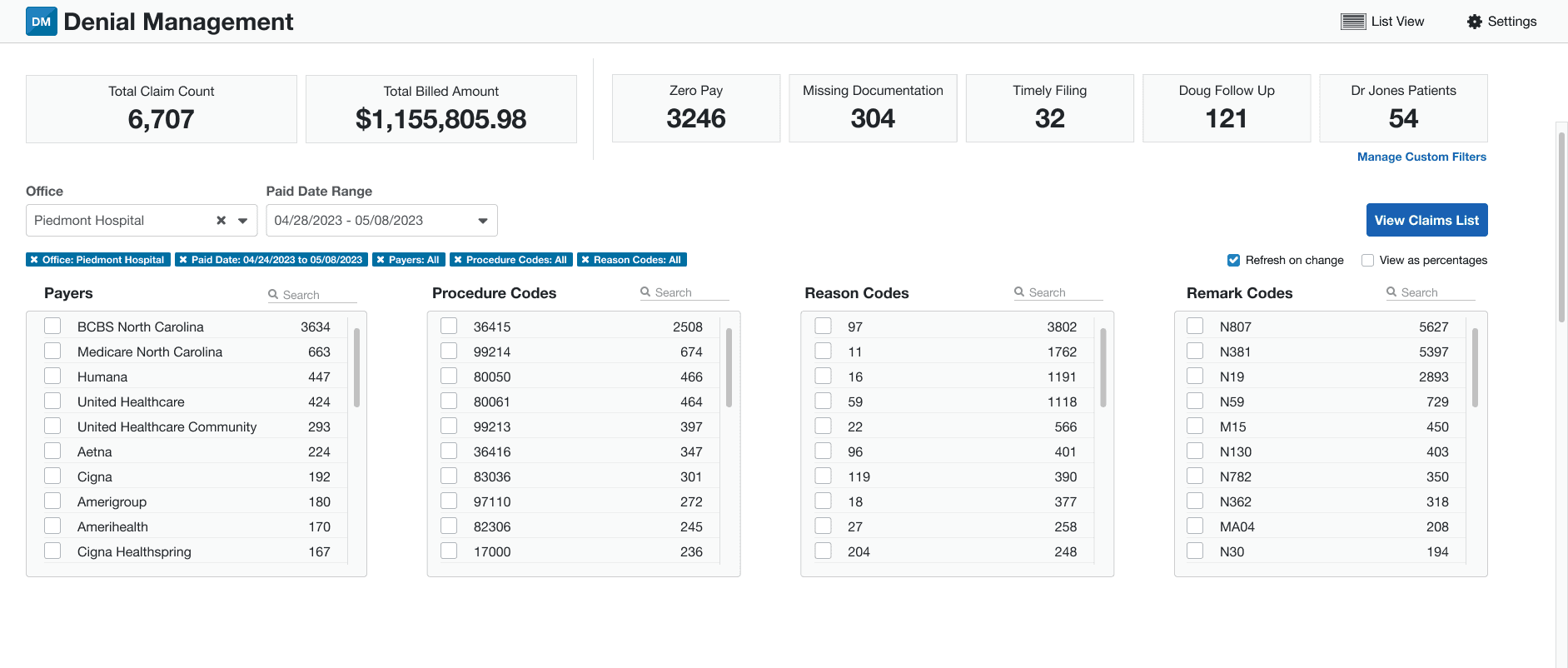
This view categorized denied claims by four attributes: payer, procedure code, reason code, and remark code.
Users can quickly identify which attributes are associated with the most denials by count and monetary value. Once they have filtered the denials down to a manageable list, they can return to the table list view to see only those claims.

We also integrated the 'Save Search' functionality into the dashboard, allowing users to quickly identify high-priority denials with reasons such as 'Zero Pay or Missing Documentation'.
Final Thoughts
In conclusion, the denial management project has yielded positive results and valuable insights. The claim detail panel and dashboard have been well received and proven to be successful, warranting their inclusion in the library for related applications. The early user interviews were instrumental in challenging the false assumption that all denied claims are equal, leading to important design and behavior changes.
While our ideal vision for the application was to have a predictive capability in identifying denied claims before submission, we encountered limitations with the current backend data structure that hindered the realization of this goal. Recognizing this roadblock later in the project, we have decided to prioritize the development of a predictive model as a future enhancement.
Overall, the denial management project has made significant progress in reducing denials and improving the efficiency of the revenue cycle. The project team's dedication and efforts have laid a solid foundation for continued enhancements and refinements in the future.
Robert Rhoden © 2023